The New Dietary Guidelines Miss the Mark
New Food Pyramid 2026…
Why Are Still Debating This?
Every five years, the Dietary Guidelines for Americans are released to help shape nutrition policy, school meals, healthcare recommendations, and how Americans think about food and health. These guidelines are supposed to reflect the best available science and translate it into practical, population-wide guidance.
That’s the intention.
The problem with the newest dietary guidance isn’t that it challenges old ideas. It’s that it lacks nuance, historical context, and balance—and when nutrition guidance is oversimplified, the public doesn’t get healthier. They get confused, polarized, and misled.
Here in this Blog we chase evidence, context, and sustainability. Ironically, much of what we promote already mirrors the strongest parts of the 2020–2025 Dietary Guidelines, with thoughtful updates where the science has clearly evolved.
The Food Pyramid Celebration: A Clear Education Gap
What’s especially troubling is watching people enthusiastically cheer the return of a “new” food pyramid—without realizing that the original food pyramid was abandoned decades ago because it failed both scientifically and practically.
The pyramid model was phased out, redesigned, and ultimately replaced by MyPlate because it was:
Overly simplistic
Poorly understood by the public
Not reflective of real eating patterns or health outcomes
Seeing people celebrate a pyramid today as if it’s a bold correction of modern nutrition only highlights a lack of education and historical context in this space. Recycling an outdated visual and calling it innovation doesn’t move public health forward—it exposes how easily nutrition messaging can be manipulated when foundational knowledge is missing.
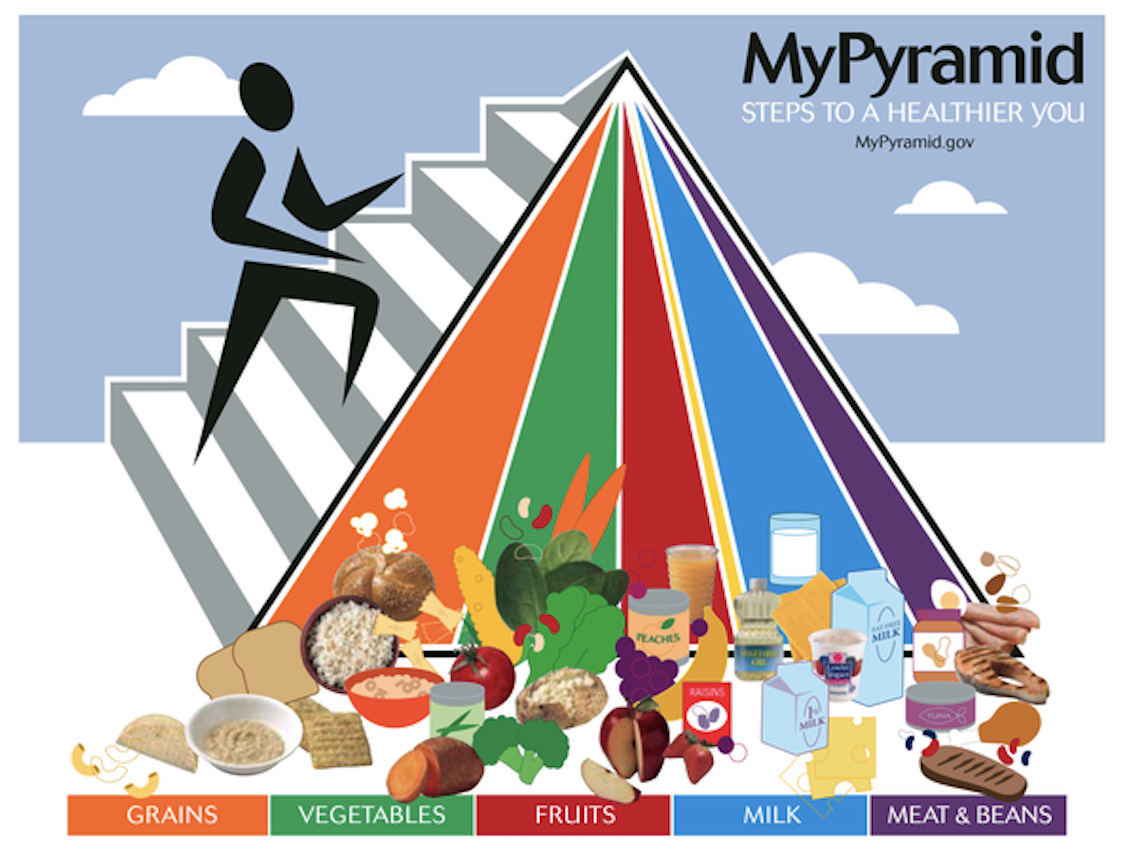
See the Pyramids Below:
Food Pyramid 1992
MyPyramid 2005
Why Dietitians Are Frustrated—and Why It Matters
Dietitians are not mad because nutrition guidance evolves.
We expect it to. We demand it!
We’re frustrated because these “new” guidelines evolved without enough depth, transparency, or respect for decades of evidence and clinical practice. And no, this isn’t a turf war—it’s a public health problem.
Let’s be honest: dietitians have been underestimated for years—and at times, we earned that reputation. Too many people experienced nutrition as a laminated handout, a food picture, and a “good luck” send-off. But that version of dietetics is outdated, lazy, and largely gone.
Modern dietitians work in chronic disease prevention, cardiometabolic health, renal disease, oncology, pediatrics, geriatrics, mental health, and whole-person care. We don’t just talk food—we talk access, behavior change, stress, sleep, culture, trauma, aging, medications, and real life. We are whole-health clinicians, not macro calculators with clipboards.
And yet, here we are again—watching oversimplified models get rebranded as bold innovation while nuance gets ignored.
For example this was promoted on HHS social media:
“HHS marked the release of the Dietary Guidelines for Americans with leaders from health, agriculture, and science, marking a reset of federal nutrition policy around nutrient density. The message is clear: eat real food.”
Calling this a “reset” around nutrient density while telling Americans to simply “eat real food” is not nutrition policy—it’s a slogan. Nutrient density without definition, structure, or guardrails invites interpretation, not better health. Americans already believe they eat real food, and this kind of vague messaging doesn’t change behavior—it reinforces existing biases and encourages overcorrection. Effective public health guidance should be clear, specific, and grounded in decades of evidence, not reduced to a bumper-sticker phrase that sounds bold but ultimately leaves people more confused than informed.
Public health guidance is not a marketing campaign. It must account for children, chronic disease risk, food insecurity, culture, aging, mental health, stress, and lifestyle—not just protein talking points and crowd-pleasing sound bites.
When confident misinformation gets applause and outdated frameworks are revived like they’re revolutionary, it exposes just how fragile nutrition literacy still is.
So to those cheering the return of the Food Pyramid and saying “it’s about time”—no. You’re not early. You’re not brave. You’re about a decade late. That argument expired years ago. Please take a seat and let evidence—not nostalgia—drive the conversation.
Why the 2020–2025 Guidelines (and MyPlate) Got More Right Than People Think
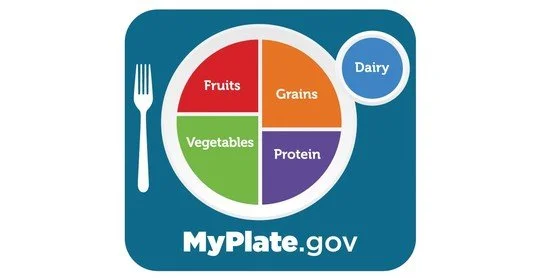
MyPlate was never meant to be perfect. It was meant to be understandable and practical in daily life.
It emphasized:
Fruits and vegetables as a foundation
Whole grains and quality carbohydrates
Adequate protein from both animal and plant sources
Dairy or fortified alternatives
Limits on saturated fat (which are still true with the new guidelines!!), sodium, added sugars, and alcohol (not so true with the new guidelines)
Most importantly, it focused on dietary patterns, not single nutrients.
That distinction matters—because health is not built by elevating one macronutrient while ignoring the rest of the picture.
Myplate 2011
The New Guidelines: Some Correct Ideas, Framed the Wrong Way
Let me be very clear: I agree with the higher protein targets in the new guidance. I always have. Many dietitians have been recommending protein intakes above the RDA for years, particularly for metabolic health, weight management, aging, and physical activity.
What I strongly disagree with is the framing—especially the claim that we are “ending the war on protein.”
There was never a war on protein.
Dietitians have always recommended an increase in protein. What we have pushed back on is:
Excessive saturated fat intake
Protein crowding out fiber-rich plant foods
Oversimplified “more protein fixes everything” messaging
That is not anti-protein. That is evidence-based nutrition.
When the Secretary of Health frames this as a battle that never existed, it signals a lack of understanding of nutrition history and clinical practice—which is deeply concerning given the influence of these guidelines. It also raises an uncomfortable question: was the science driving the message, or was the message shaped to fit a narrative already supported by cattle and dairy industry interests?
I also wrote a blog on Protein just a few weeks ago, find it here: Protein Drama
The Chasing Your Health (CHY) Plate
This is the way I feel the guidelines image should have been revamped. Yes—protein deserves a larger role on the plate than traditional MyPlate visuals suggested. That’s why Chasing Your Health promotes a rebalanced plate, not a pyramid and not a single-nutrient obsession.
The CYH Plate
~⅓ protein
Lean animal proteins (fish, turkey, chicken), eggs, dairy, legumes, tofu, or a mix~⅓ vegetables and fruit
Fiber, micronutrients, gut health, disease prevention~⅓ quality carbohydrates
Whole grains, starchy vegetables, legumesHealthy fats and dairy (or alternatives) based on the individual
*And the good news is this can and should be adjusted depending on what your goals are. This is meant to be a guide not a “do this or die from chronic disease”.
This structure reflects what we see clinically every day: adequate protein and fiber improves satiety, preserves lean mass, supports glycemic control, and helps people actually sustain healthy eating patterns.
This isn’t extreme. It’s realistic.
The Chasing Your Health Plate
Why the Protein RDA Was Never Meant to Be the Goal
The current protein Recommended Daily Allowance (RDA) of 0.8 g/kg/day has always been misunderstood.
That number was established to maintain nitrogen balance.
What Nitrogen Balance Means
Nitrogen balance compares:
Nitrogen in (from protein intake)
Nitrogen out (urine, stool, sweat, skin)
Being in nitrogen balance simply means: You are not actively losing body protein.
It does not represent optimal muscle mass, metabolic health, recovery, or healthy aging.
The RDA is a minimum threshold, not a performance or longevity target. That’s why modern evidence consistently supports protein intakes closer to 1.2–1.6 g/kg/day for many adults.
So yes—I agree with the new protein numbers.
I just reject the idea that this discovery is new or that dietitians were ever opposed to it.
Nutrition Is Young—and It Changes (Eggs Are Proof)
Nutrition science evolves because research methods improve.
Eggs were once vilified for cholesterol, later re-evaluated with stronger population data, and are now understood as a nutrient-dense, affordable protein for most people.
Were eggs ever truly “bad”? No.
Our understanding was simply incomplete.
The same evolution applies to dairy fat.
Full-Fat Dairy: Context Still Wins
Earlier guidelines favored low-fat dairy largely due to saturated fat concerns. Newer research shows the story is more nuanced.
We now know:
The food matrix matters
Fermented dairy behaves differently than ultra-processed foods
Saturated fat cannot be evaluated in isolation from dietary pattern
The CYH Take
Full-fat dairy isn’t the villain—but it’s not a free-for-all either. When you tell a population that already struggles with portion control that full-fat foods are “back,” most people don’t hear nuance—they hear permission. And Americans don’t swap foods, they add them.
Praising full-fat dairy without guardrails leads to more cheese, more butter, more calories, and—surprise—more saturated fat. “Less processed” doesn’t magically cancel basic physiology, and excess is still excess.
This is the real problem with the new guidelines messaging: nutrition advice without education doesn’t empower people—it sets them up to overdo it.
Again: context beats ideology.
Physical Activity: Any Movement Counts
Health is not built on nutrition alone. Physical activity is a critical pillar of health and deserves to be acknowledged alongside dietary guidance—even if briefly. While these are Dietary Guidelines, nutrition and movement are not mutually exclusive. Ignoring physical activity in the conversation misses a key driver of long-term health.
Yes, the guidelines say:
150+ minutes per week
~30 minutes most days
A mix of cardio, strength, and movement
But here’s the part people forget: any activity is good activity.
Movement that actually matters includes:
Walking or jogging
Yardwork and gardening
Housework
Taking the stairs
Grocery shopping
Activities of daily living (ADLs)
Consistency beats perfection every time. I tell patients daily: find movement you enjoy—or sneak it in where you can (park farther away, take the long route, stand more). It all counts.
And a quick reality check: getting your workout in doesn’t cancel out the other 23 hours. In college we called this being an “active couch potato”—you exercise, then spend the rest of the day sitting. The goal is simple: move more across your entire day, not just during your workout.
Chasing Your Health Bottom Line
We are not team “old guidelines” or team “new guidelines.”
We are team:
Protein forward—with context
Plant inclusive—not plant exclusive
Dairy with nuance
Movement that meets people where they are
Science over slogans
You can prioritize protein without ignoring fiber.
You can support dairy without dismissing saturated fat science.
You can improve nutrition guidance without rewriting history.
That’s not political.
That’s responsible nutrition. And it’s exactly what Chasing Your Health will continue to stand for.